Introduction
An ACL (anterior cruciate ligament) injury is often considered a surgical condition—especially for athletes or highly active individuals. But recent research is challenging this belief. Could non-surgical, conservative treatment be a viable and sometimes better option?
In this blog, we explore the evidence, emerging protocols like the Cross Bracing Protocol (CBP), patient classifications, and when surgery is or isn’t necessary.
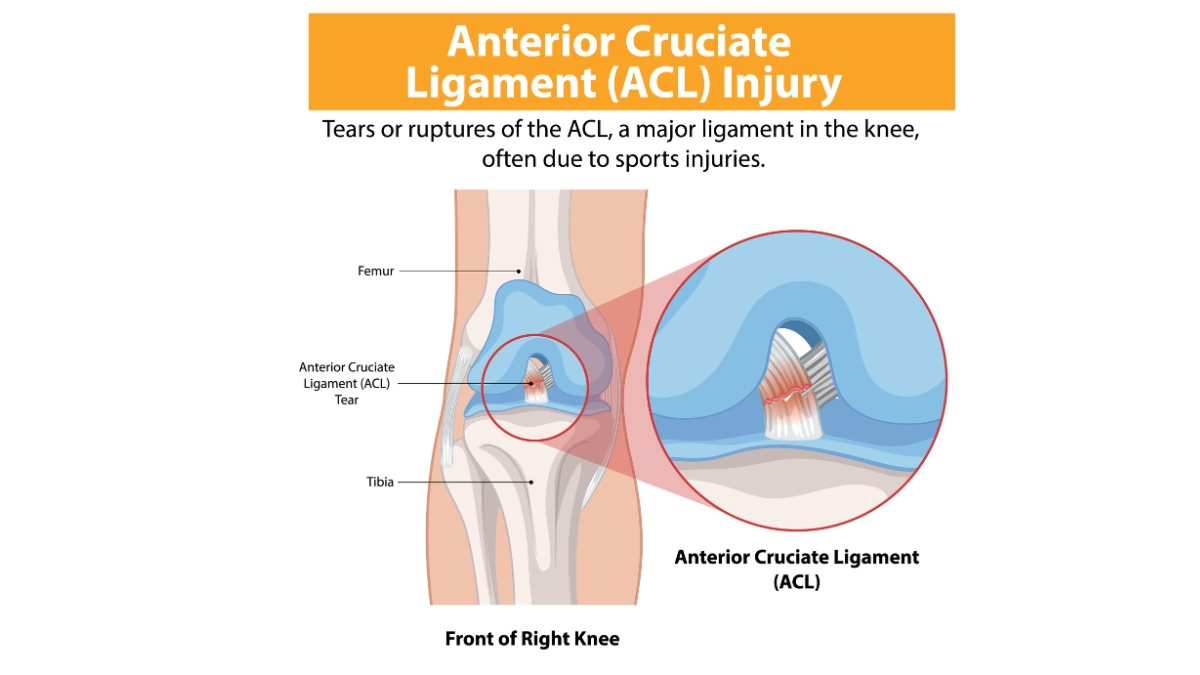
Why Take ACL Injuries Seriously?
Takeaway 1:
ACL injuries are not minor. If left untreated or poorly managed, they can lead to long-term consequences like chronic pain, instability, reduced mobility, and early-onset osteoarthritis. Early evaluation and guided intervention are critical.
Is Surgery Always the First Step?
Traditionally, ACL reconstruction surgery has been the gold standard—especially for those engaged in high-risk sports involving cutting, pivoting, or sudden direction changes. However, modern physiotherapy-led research suggests some patients can regain function without surgery.
Key Insight:
Studies now indicate that with structured rehabilitation and proper bracing, even torn ACLs can demonstrate spontaneous healing, allowing individuals to return to everyday or even sporting activities.
Real-Life Highlight: When Surgery Was Delayed—and Paid Off
A 30-year-old recreational runner experienced an ACL tear while trekking. Imaging confirmed an isolated ACL injury with no associated cartilage or meniscus damage. Guided by a physiotherapist, she underwent 12 weeks of the Cross Bracing Protocol combined with neuromuscular rehab. By the end of 6 months, she had regained stability and returned to moderate trekking—without surgery.
This is not every patient’s story, but it highlights that in specific cases, conservative management can be successful.
What Is the Cross Bracing Protocol (CBP)?
The Cross Bracing Protocol is a conservative treatment method in which the knee is immobilized in a specific angle using a custom brace. The bracing creates ideal healing conditions for the ACL, often combined with a structured physiotherapy plan.
A 2024 study by Haeringen et al. reported a 90% ACL healing rate by the third month in patients undergoing this protocol.
When Is CBP Most Effective?
CBP is most effective in cases of:
- Isolated ACL injuries
- Early intervention (within a few weeks of injury)
- No additional damage to the meniscus, cartilage, or other ligaments
MRI and clinical evaluation are essential before deciding on this route.
Surgery vs. Conservative Management: A Side-by-Side Comparison
Criteria | Surgical Management | Conservative (CBP + Rehab) |
Recovery Time | 6–9 months (with surgery + rehab) | 4–6 months (depends on progress) |
Costs | Higher due to surgery, hospital stay | Lower (rehab + bracing) |
Invasiveness | Surgical procedure | Non-invasive |
Risk of Re-injury | Exists, especially if rehab is skipped | Exists, but lower in successful CBP |
Osteoarthritis Risk | Present | Present (no conclusive difference) |
Suitable For | Athletes, high-risk movers | Low-activity individuals, isolated ACL |
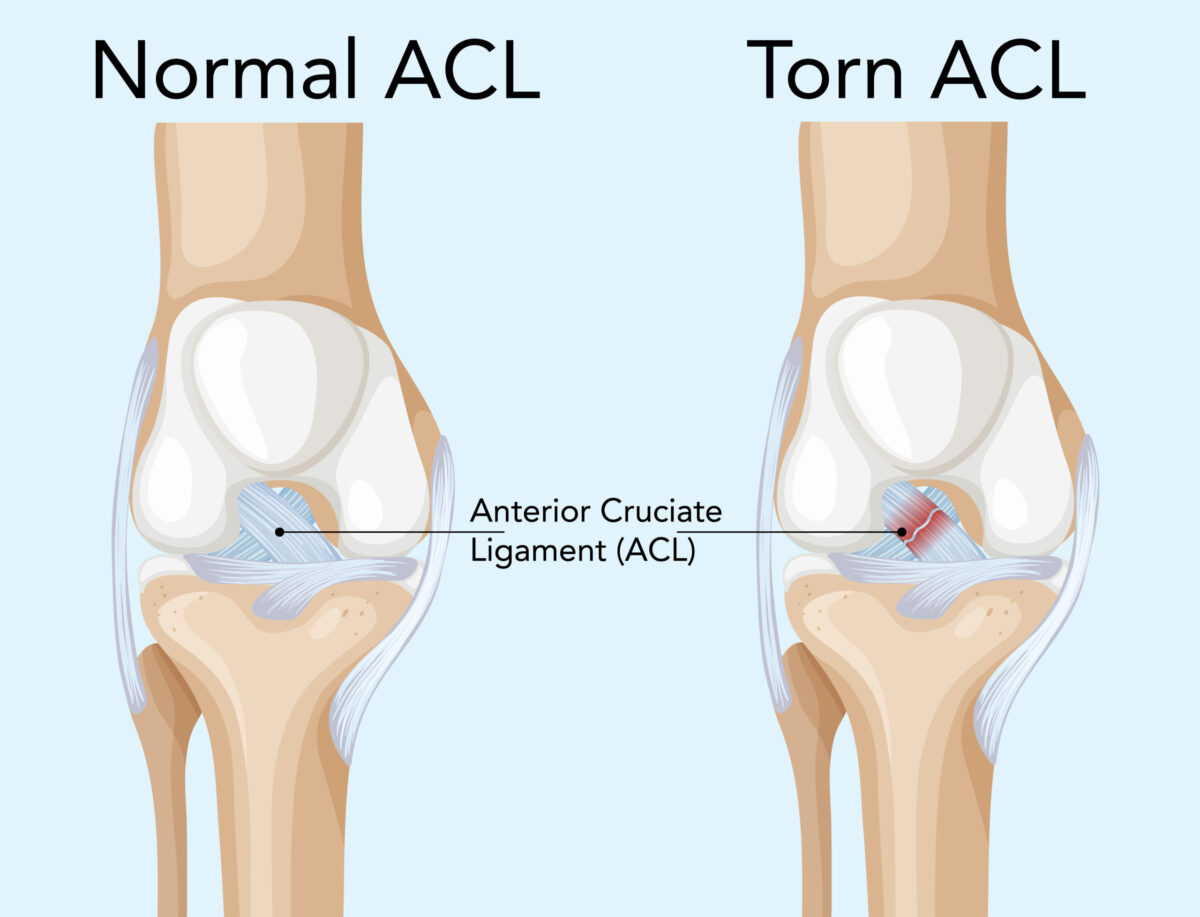
How Do I Know It’s an ACL Tear?
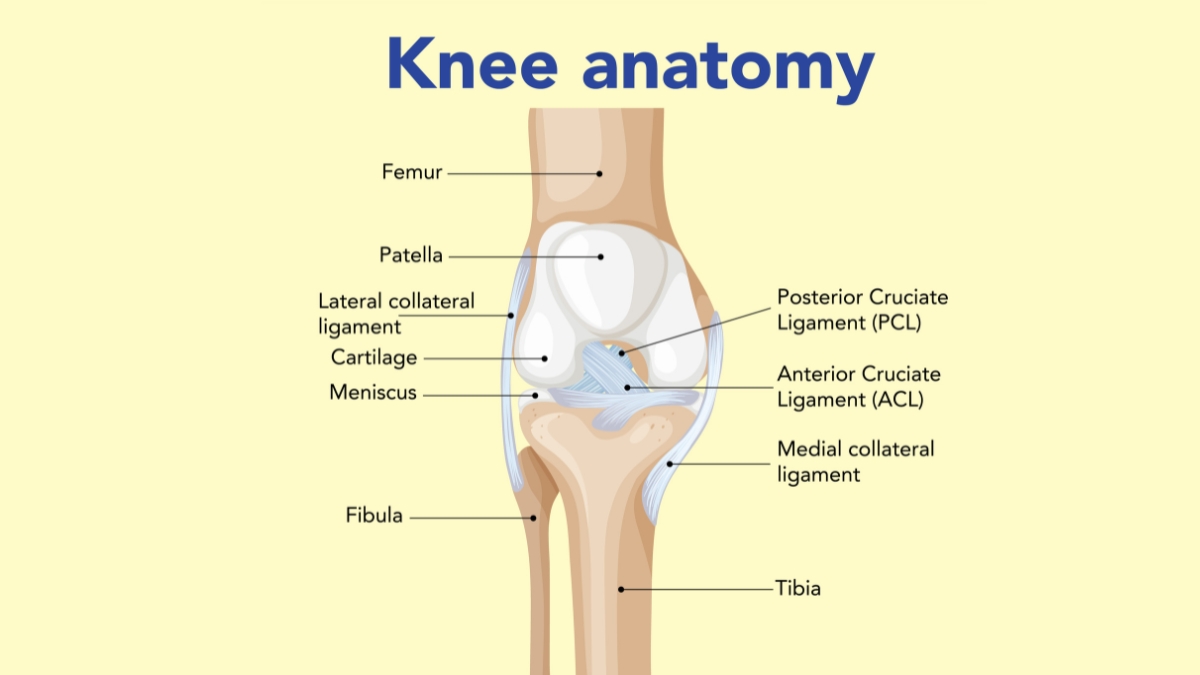
ACL injuries can mimic other types of knee trauma, such as meniscus tears or MCL injuries.
Common Signs of an ACL Tear:
- A popping sound at the time of injury
- Immediate or delayed swelling
- Knee giving way or instability
Difficulty bearing weight or extending the leg fully
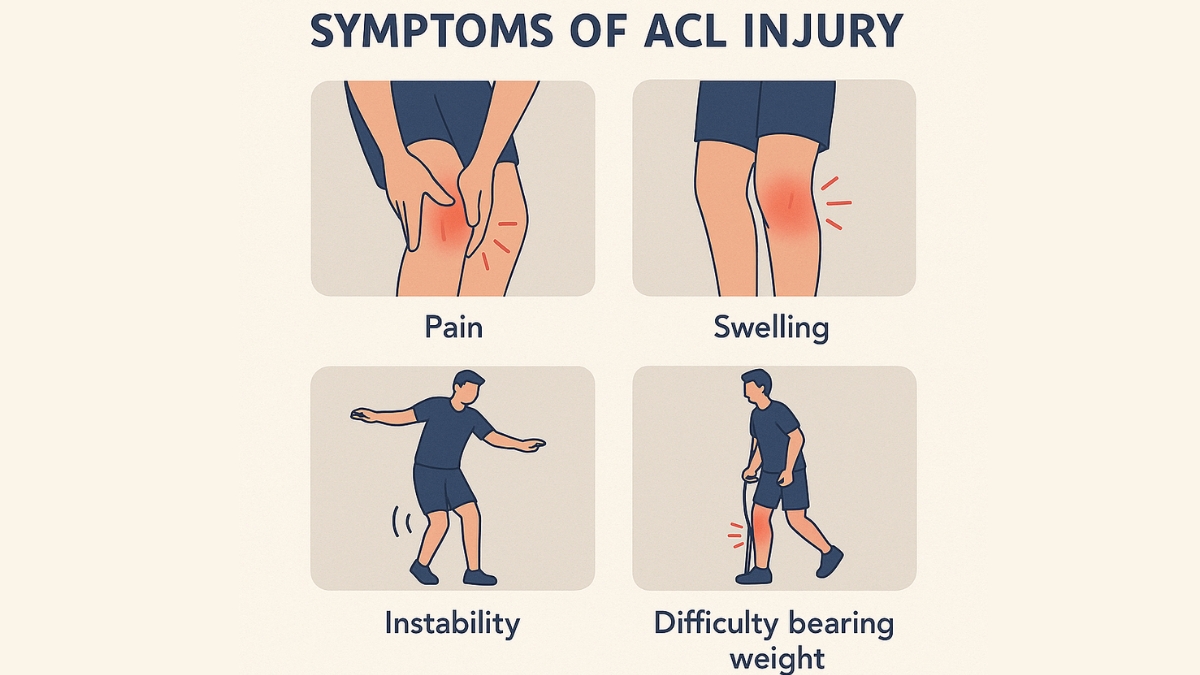
Takeaway 2:
Only a trained orthopedic or sports specialist, supported by clinical tests and MRI imaging, can confirm if it’s an ACL tear or a different knee issue. Do not rely solely on symptoms.
Understanding Recovery Profiles: Copers, Non-Copers, and Adapters
Classifying the injury and patient profile helps tailor treatment:
- Copers: Can function normally and return to activity without surgery.
- Non-Copers: Struggle with instability despite rehab and may require surgery.
- Adapters: Modify or reduce activity levels to avoid symptoms.
What About the Risk of Osteoarthritis?
Surprisingly, current research shows no major difference in early osteoarthritis risk between those who undergo ACL surgery and those who don’t. In fact, higher risk is often associated with:
Poor movement patterns
High activity levels
Improper rehab (regardless of treatment type)
Can You Delay Surgery?
Yes. Choosing conservative management doesn’t mean surgery is off the table forever. Delayed ACL Reconstruction is a proven strategy, allowing patients to:
- Build strength and coordination
- Improve neuromuscular readiness
- Potentially achieve better post-surgical outcomes
Takeaway 3:
Whether to go ahead with surgery or not is a clinical decision. Never self-decide based on internet sources or advice from peers. Consult an orthopedic surgeon or sports rehab expert who can assess your individual case.
Conclusion: Treat Early, Treat Smart
ACL injuries are serious, but surgery isn’t always the first or best option. With early diagnosis, imaging, structured rehab, and emerging techniques like the Cross Bracing Protocol, many individuals—especially non-athletes—can regain function without surgery.
That said, conservative treatment is not for everyone. Your long-term recovery and knee health depend on:
- Early consultation
- Personalized care
- Following rehab diligently
Making informed, collaborative decisions with your care team.


