Introduction: The Growing Burden of Knee Pain in India
In the Indian clinical landscape, knee pain has transitioned from being a hallmark of aging to a pervasive musculoskeletal challenge affecting diverse age groups. The confluence of a rapidly aging population, a sedentary urban lifestyle, and a metabolic syndrome epidemic has created a significant burden on the healthcare system.
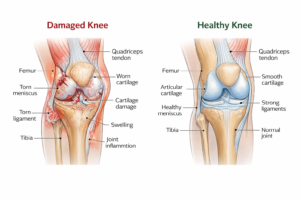
The primary challenge in India is not merely the prevalence of knee pathology, but the cultural tendency toward “therapeutic nihilism”—the belief that knee pain is an inevitable part of life. This often leads to delayed presentation, where patients seek specialist consultation only when they have reached end-stage joint destruction. Such delays transform manageable conditions into complex surgical requirements, often resulting in avoidable disability and diminished quality of life. Differentiating knee pain early is not just a clinical necessity; it is a preventive strategy to preserve joint longevity.
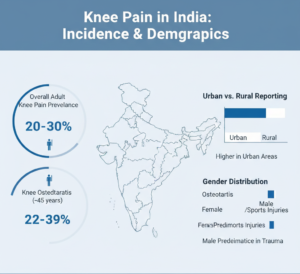
Epidemiological Landscape: Incidence and Regional Patterns
Conservative estimates suggest that the prevalence of knee osteoarthritis (OA) in India ranges between 22% and 39%. However, the spectrum of knee pain extends far beyond degenerative changes.
Regional Variance: Studies indicate higher reporting of knee-related complaints in urban clusters, likely due to higher BMI and sedentary habits. Northern and Southern India report significant numbers, often influenced by dietary habits and metabolic predispositions.
Gender Disparity: Females exhibit a significantly higher prevalence of osteoarthritis, often presenting earlier (in their late 40s) compared to males. This is attributed to post-menopausal hormonal shifts, smaller joint surface areas, and biomechanical factors.
Male Predominance in Trauma: Conversely, males show a higher incidence of trauma-induced knee pain, largely driven by road traffic accidents (RTAs) and sports-related ligamentous injuries.
Age-Wise Classification of Knee Pain
Understanding the patient’s age is the first step in narrowing the differential diagnosis.
1. Children and Adolescents (Below 20 Years)
Pain in this group is often related to growth or mechanical alignment.
Osgood-Schlatter Disease: Traction apophysitis of the tibial tubercle.
Patellar Instability: Often linked to generalized ligamentous laxity.
Congenital Deformities: Early detection of Genu Varum (bow legs) or Genu Valgum (knock knees).
2. Young Adults (20–40 Years)
This demographic is the “active” cohort, where pain is usually acute or overuse-related.
Ligamentous Injuries: ACL, PCL, or MCL tears following sports or trauma.
Meniscal Injuries: Often presenting with mechanical symptoms like locking.
Patellofemoral Pain Syndrome (PFPS): Common in desk-bound professionals beginning sudden exercise regimes.
3. Middle-Aged Adults (40–60 Years)
This is the “transition phase” where degenerative changes begin to surface.
Early Osteoarthritis: Medial compartment wear is common in the Indian population.
Degenerative Meniscal Tears: Occurring without a specific traumatic event.
Obesity-Related Overload: Increased joint reactive forces leading to chronic synovitis.
4. The Elderly (60–70+ Years)
Advanced Osteoarthritis: Characterized by joint space obliteration and osteophyte formation.
Post-Surgical Pain: Evaluation of previous interventions.
Secondary Causes: Crystal arthropathies (Gout/CPPD).
Gender-Specific Patterns and High-Risk Groups
Gender-Wise Predisposition
Females: Factors include a wider Q-angle (pelvic width to knee alignment), which increases stress on the patellofemoral joint, and lower bone mineral density. Conditions like PFPS and Osteoarthritis are predominant.
Males: Higher risk for high-energy trauma, occupational meniscus wear in manual laborers, and secondary OA following neglected ligamentous injuries.
High-Risk Groups Requiring Immediate Orthopedic Scrutiny
Limb Deformities: Patients with pre-existing bow legs or knock knees develop eccentric loading, leading to rapid compartmental wear.
Post-Polio Residual Paralysis (PPRP): These patients have unique biomechanical stresses and muscle imbalances that accelerate joint degeneration.
Prior Surgery/Implants: Any patient with a history of internal fixation (rods/plates) near the knee or previous ligament reconstruction who develops new pain must be referred to rule out implant irritation, infection, or hardware failure.
The Obese Patient: Excess weight acts as a chronic mechanical stressor and a pro-inflammatory stimulus.
Clinical Insight: The Surgeon’s Perspective
Expert Comment – Dr. Pradeep Kochappan, Senior Orthopaedic & Sports Knee Surgeon:
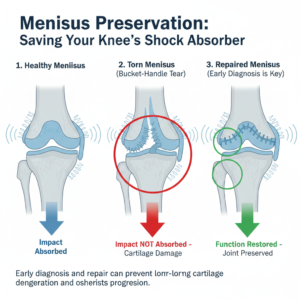
“The ‘wait and watch’ approach is the enemy of joint preservation. In young athletes or active adults, a meniscus tear is not just a source of pain; it is the loss of a vital shock absorber. Early diagnosis and meniscus preservation through repair—rather than resection—can delay the onset of osteoarthritis by decades. We must move away from the idea that every knee pain in a 40-year-old is ‘just age’ and look deeper for structural injuries that are salvageable.”
Structured Diagnostic Approach for GPs and PhysiotherapistsA systematic evaluation prevents the pitfalls of “symptomatic-only” treatment.
1. Focused History
Onset: Was it a “pop” (ACL), a “twist” (Meniscus), or “insidious” (OA)?
Mechanical Symptoms: Does the knee lock, catch, or give way?
Surgical History: Are there implants? Was there a prior arthroscopy?
2. Physical Examination
Effusion: Check for intra-articular swelling (Wipe test/Patellar tap).
Range of Motion (ROM): Loss of terminal extension is a red flag for mechanical blocks.
Joint Line Tenderness: A hallmark of meniscal pathology.
3. Imaging Strategy
X-ray (Weight-bearing): Essential for assessing joint space. Non-weight-bearing films are often misleading in early OA.
MRI: Indicated when soft tissue injury (ligament/meniscus) is suspected or when X-rays are normal but pain is recalcitrant.
Note: Do not treat the “MRI report”; treat the patient. Many asymptomatic individuals have degenerative MRI findings.
Clinical Decision Pathway for Knee Pain
By Dr. Viresh Murugodi
Patient Presents with Knee Pain
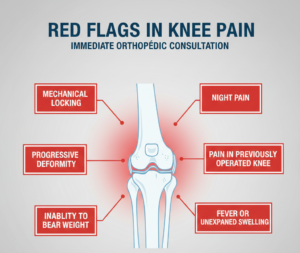
Screen for Red Flags: (Fever, night pain, trauma, locking, previous surgery).
If Yes: Immediate Orthopedic Referral.
Assess Age:
< 40 Years: Evaluate for trauma/instability. If clinical tests (Lachman/McMurray) are positive $\rightarrow$ MRI & Specialist Consultation.
> 60 Years: Obtain weight-bearing X-rays.
Interpret Findings:
Normal X-ray/Mild OA: Trial of structured physiotherapy (4-6 weeks) and lifestyle modification.
Severe Deformity/Bone-on-Bone: Orthopedic Consultation for surgical evaluation.
Presence of Implants/Hardware: Do not attempt aggressive PT; Refer to Surgeon.
Re-evaluation: If no improvement in 4 weeks of conservative care $\rightarrow$ Specialist Referral.

When NOT to Treat: Mandatory Referral Scenarios
Physiotherapists and General Practitioners must identify cases where conservative management is contraindicated or risky:
Presence of Orthopedic Implants: Pain around a plate, screw, or nail requires an X-ray to check for loosening or “stress shielding.”
Mechanical Locking: A “locked” knee usually signifies a displaced bucket-handle meniscus tear or a loose body. Forcing ROM in these cases can cause permanent cartilage damage.
Progressive Deformity: If the “gap” between the knees is visibly increasing.
Inability to Bear Weight: Following an injury, this suggests a fracture or high-grade ligamentous disruption.
Night Pain or Unexplained Swelling: Must rule out inflammatory arthropathy or neoplastic processes
Clinical Insight: The Surgeon’s Perspective
Expert Comment – Dr. Viresh Murugodi, Senior Knee Replacement and Arthroscopy Specialist:
“A structured referral pathway is the backbone of successful knee care. We frequently see patients who have undergone months of physiotherapy for ‘stiffness’ when they actually had a mechanical block from a torn meniscus or a loosening implant. The goal of the GP or PT should be to identify these ‘surgical outliers’ early. Timely intervention, such as a partial knee replacement or an arthroscopic fix, is far more successful than salvage surgery performed too late.”
Current Advances in Management
Knee care has moved beyond simple “rest and analgesics.”
Modern PT: Focuses on neuromuscular control and vastus medialis obliquus (VMO) strengthening.
Biologicals: Image-guided injections (PRP or Viscosupplementation) for early-to-moderate OA.
Robotic & Navigation Surgery: Increasing precision in Total Knee Arthroplasty (TKA).
Partial Knee Replacement (UKA): A bone-preserving surgery for patients with isolated medial compartment OA.
Patient-Centric FAQs
Is knee pain a normal part of aging?
No, while wear occurs, pain that limits activity is not “normal” and needs evaluation.Can I rely only on an X-ray?
X-rays show bones; they don’t show ligaments or early meniscus tears. If pain persists despite a “normal” X-ray, further imaging is needed.Does a meniscus tear always need surgery?
Not always, but “locking” or “catching” usually does.Can physiotherapy worsen my pain?
If there is a mechanical block (like a torn meniscus), aggressive exercise can aggravate the injury.When is surgery unavoidable?
When conservative measures fail, deformity is progressive, or daily quality of life is severely compromised.What are ‘Red Flags’?
Fever, sudden swelling, inability to walk, or the knee getting stuck.Why do my knees click?
If painless, it’s usually benign. If accompanied by pain, it indicates a structural issue.Is walking good for knee pain?
In moderation and on flat surfaces, yes. Avoid stairs and squats if pain is acute.What if I have old rods/plates in my leg?
Any new pain must be checked by a surgeon to ensure the hardware isn’t failing.Do I need an MRI for every pain?
No, only if clinical examination suggests a soft-tissue injury.Are knee injections helpful?
They provide temporary relief in early stages but don’t “cure” advanced OA.Can obesity cause knee pain?
Yes, losing 5kg can significantly reduce the load on your knees.What is a ‘Partial’ knee replacement?
It replaces only the damaged part, preserving healthy bone and ligaments.How long is the recovery after ACL surgery?
Usually 6-9 months for full sports return.What is ‘Locking’ of the knee?
It’s when you physically cannot straighten the leg. This is an emergency.Is ‘Gout’ a cause of knee pain?
Yes, it causes sudden, severe swelling and redness.Can children get serious knee issues?
Yes, growth-plate injuries or ligament tears can occur in young athletes.Why do women get more knee pain?
Due to wider hips, different muscle strengths, and hormonal changes.What is ‘Knock Knees’?
When the knees touch but the ankles stay apart; it can lead to outer-knee wear.Should I wear a knee cap?
It provides support but doesn’t fix the underlying cause; use it only as a temporary aid.
Conclusion
Differentiating knee pain requires a shift from viewing it as a solitary symptom to understanding it as a manifestation of specific structural or mechanical failures. In the Indian context, where delayed diagnosis is a significant hurdle, the role of the General Practitioner and Physiotherapist as the first line of defense is paramount.
By applying age-based logic, recognizing red flags, and adhering to a structured referral pathway, we can ensure that patients receive the right intervention at the right time. Collaborative care between the primary care provider and the orthopedic specialist is the only way to stem the rising tide of knee-related disability in our society.



